Did you know that there are over 100 autoimmune conditions? Autoimmune conditions have become more prevalent, are often misdiagnosed, and each needs to be looked at differently. Functional medicine is different from conventional or standard medicine and looks for the root cause of an autoimmune disorder rather than just the symptoms. Regardless of the tissue or gland that is impacted by an autoimmune disease, many autoimmune disorders share the same issues at the core. For example, in Hashimoto’s disease the thyroid is viewed as the problem gland, whereas the joints are the culprit in rheumatoid arthritis. But actually, Hashimoto’s disease and rheumatoid arthritis have a lot in common. They are both characterized by a dysfunctional immune system and they may both be driven by the very same underlying causes.
Understanding Autoimmunity
Your immune system’s job is to protect you by fighting off infections, and tolerating friendly microbes and harmless substances such as food. Your immune system begins working on day one. It develops according to your genetics and external factors such as how you were born, if you were breastfed, and how healthy your mother was. In the beginning, much of the early immune response is dependent on the mother’s transfer of antibodies until her baby is strong enough to develop its own immune response.
Autoimmunity means that the immune system mistakenly attacks and damages one’s own tissues. Attacking tissues, organs, and cells. Why? There are several reasons why this happens and why functional medicine examines the root causes, not just symptoms alone.
I always remind people that the body is intelligent. The autoimmune process isn’t wrong, it’s your body’s way of trying to defend you. Symptoms and an autoimmune diagnosis mean that your body is trying to deal with a dysfunction. It thinks it is under attack. If you have an autoimmune disease, the next step is to figure out why your body thinks it is under attack. Once you and your functional medicine practitioner figure out the root causes and address them, it will turn off the autoimmune process and get you back on a path to wellness.
Keep reading to learn the nine main causes of autoimmunity that we address in our clinic on a daily basis.
An Imbalanced Immune System: Th1 and Th2
In autoimmune disorders, there is an imbalance in the immune system. One side is typically more active than the other. T helper cells (also known as CD4+ cells) are immune cells that protect the body. They “help” other immune cells fight foreign invaders by secreting chemical messages, called cytokines. Th1 (type I helper T lymphocytes) help to fight viruses and bacteria that invade our cells. Th2 (type II helper T cells) help defend us from larger organisms such as parasites. Another T helper cell, Th17, protects the body from pathogens. However, it can be destructive if not well controlled. Other T cells, called regulatory T cells, counteract the others. Treg cells help to keep the peace so that the body can tolerate harmless substances from the outside world and Tregs prevent autoimmune disease.
When these T cells are imbalanced, they can cause dysfunction. Although overly simplified, Th1 is more associated with the “natural killer cells” that help your body fight off pathogens while Th2 response can promote the development of antibody producing cells. When Th2 is overactive (and Th1 is down), it can lead to allergies or asthma. When Th1 is weak it can allow for chronic infections in the body. Th1 also helps suppress an overactive Th17 response. When Th17 ramps up it can lead to tissue destruction, whether to the thyroid, joint, skin, gut or any tissue in the body. An unchecked Th17 response is associated with the tissue destruction that happens in autoimmunity.
The goal in functional medicine is to restore balance to the immune system by figuring out the underlying problems and addressing them.
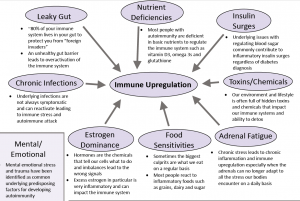
Root Causes of Autoimmune Conditions
- Leaky gut
- Insulin surges
- Mental and emotional stress
- Adrenal fatigue or HPA axis dysfunction
- Chronic infections
- Environmental toxins/chemicals
- Food sensitivities
- Nutrient deficiencies
- Estrogen dominance
1. Leaky Gut
Did you know that “80% of your immune system lives in your gut”? This is so your gut can protect you from “foreign invaders.” Intestinal permeability, also called leaky gut, happens when the cells in your gut spread apart, “leaking” larger molecules from the gut into the bloodstream, where they don’t belong. These large molecules may trigger inflammation in the body and brain, causing tissue damage. Leaky gut has been highly associated with autoimmunity and most people with autoimmune disorders have leaky gut. In fact, some researchers believe leaky gut is a critical step in triggering autoimmunity in the first place. The large molecules that pass through may be non-digested food proteins, viruses, bacteria, fungi, parasites, toxins or chemicals. The immune system will begin to attack these proteins and think they are dangerous. Leaky gut can also lead to multiple food sensitivities.
2. Insulin Surges
Whether or not you have diabetes, underlying issues regulating blood sugar at normal levels can result in inflammatory insulin surges. Insulin is a hormone that naturally occurs in the body to support normal blood sugar levels. When your sugar levels increase, insulin is released to help your cells use the sugar for energy. It also stores excess sugar to use later on. Spikes of blood sugar or low blood sugar can lead to immune system problems because insulin surges are inflammatory. Most people in the United States are eating far too much sugar and refined carbohydrates (think of packaged foods like chips, crackers, pasta, bread, cookies, cakes, and more), which causes blood sugar dysfunction. Healthy protein, fats, and complex carbohydrates throughout the day are important for maintaining stable blood sugar and insulin levels.
Insulin resistance, which is often seen with low-grade inflammation, suppresses anti-inflammatory Treg cells, and can promote Th1/Th2 immune imbalance. Insulin resistance is much more common than you think. One in ten Americans has diabetes; while one in three has prediabetes. And insulin resistance is usually present for years before blood sugar changes are first seen on lab tests.
3. Mental and Emotional Stress
Mental and emotional stress cause physical changes in the body. It activates the sympathetic nervous system response, which is intended to protect us and keep us alive. However, with excess mental stress, the nervous system “learns” to always be on guard and in survival mode.
In the Adverse Childhood Experiences study, there was a correlation between mental and emotional traumas in childhood and increased risk for autoimmunity and other chronic health conditions down the road. This increased chance of developing autoimmunity has been replicated in studies of chronic stress and in those with trauma or intense stress.
4. Adrenal Fatigue
Chronic stress can lead to adrenal fatigue, or hypothalamic-pituitary-adrenal axis dysfunction, which in turn leads to chronic inflammation and autoimmunity. The adrenal glands produce the stress hormone, cortisol, as part of your “fight or flight” response. When your stress levels rise, your sympathetic nervous system turns on, and the adrenal glands release cortisol. The stress response is best suited to short bursts of occasional stress, such as an elk running away from a lion. Normally in acute stress, the pro-inflammatory effect of the sympathetic nervous system and the anti-inflammatory effect of cortisol cancel each other out. The net result is no inflammation. But if we are stressed all day, every day, and cortisol is chronically high, cortisol receptors stop working as effectively and cortisol loses its anti-inflammatory power. The net result of chronic stress is inflammation.
High stress and high cortisol also lead to an unhealthy microbiome, leaky gut, food sensitivities, as well as blood sugar/insulin issues and poor sleep. It also can deplete the precursor hormone, progesterone, causing estrogen dominance. All of these different mechanisms can contribute to the autoimmune process.
5. Chronic infections
Infections can be caused by bacteria, viruses, fungi, or parasites. These are just a few that can be triggers for autoimmunity:
Intestinal dysbiosis – your large intestines have an overgrowth of bad bacteria, fungus, parasites, or there aren’t enough good bacteria. There is a close interaction between your gut microbiome and autoimmune disease.
SIBO or small intestinal bacterial growth – Overgrowth of gut bacteria from your large intestines getting into your small intestines is known as SIBO. SIBO is common in autoimmune diseases such as inflammatory bowel disease, scleroderma, celiac disease, and Hashimoto’s hypothyroidism.
Candida albicans – Candida is a common fungus that can grow out of control in vulnerable people, especially with a high sugar diet. Candida overgrowth can cause fatigue, brain fog, or gut symptoms.
6. Environmental Toxins and Chemicals
Our immune system can be greatly affected by the toxins and chemicals we encounter in our environment.
Environmental triggers can break down our oral tolerance which in turn changes the microbiota in our guts, this can enhance gut permeability to large molecules and cause autoimmunity. Remember leaky gut? Toxins, diet, infections, and genetics all play a role in leaky gut and immune upregulation. Toxins stimulate the immune response and can result in chronic inflammation and a mistaken autoimmune attack on your tissues.
Some of the toxins and chemicals that can trigger autoimmune disease include:
- Drugs and medications
- Silica
- Asbestos
- Adulterated rapeseed oil
- Iodine
- Trichloroethylene
- Metals and heavy metals
- TCDD
- Dioxin
- Pesticides
- Fungicides
- Mineral oil
- Cosmetics
- Artificial sweeteners
- Monosodium glutamate (MSG)
- Household products
7. Food Sensitivities
Many people react to inflammatory foods such as grains, dairy, and sugar but they don’t realize it. Functional medicine doctors look at the diet to identify food triggers of autoimmune disorders. These include rice, wheat, corn, eggs, dairy, nuts, seeds, and nightshade vegetables (tomatoes, peppers, and eggplants). Even sweeteners such as fruit and sugar can trigger an autoimmune process. Food sensitivities can be tricky to figure out because food sensitivities are often delayed. Symptoms of a food sensitivity may not show up until hours, or even days, later.
Food sensitivities are not the same as food allergies. An allergy is an immune reaction to a specific food. Reactions usually occur right away after exposure and can be severe and life-threatening to some.
Food intolerances are not an immune reaction, but rather an “inability” to digest. For example, lacking the digestive enzymes to break down the sugar in milk (lactose intolerance) or the inability of the liver to process things like caffeine or alcohol. Common food intolerances include things like histamines, preservatives (such as sulfites), and lectins (the part of the plant that protects itself from being digested). Food intolerances cause inflammation in the body leading to problems like discomfort and pain.
8. Nutrient Deficiencies
Nutrition is imperative to a healthy immune system. While whole foods are the best way to obtain nutrients, sometimes supplements can be helpful to make sure you are filling any nutritional gaps. Some of the key nutrients that can balance an overactive immune response and halt tissue damage include:
Vitamin D – many people diagnosed with autoimmune disorders have vitamin D deficiencies. Vitamin D can help support a healthy immune response and may help increase T cell circulation.
Glutathione – known as the master antioxidant, it can help rid the body of toxins, chemicals, and heavy metals. Low levels of glutathione can be caused by a variety of factors, including poor nutrition, stress, aging, and environmental toxins. Glutathione reduces oxidative stress, protects against cell damage, supports Treg cell function, and helps with insulin resistance.
Omega -3 and Omega-6 Fatty Acids – These are essential fats that everyone needs. They cannot be made in the body – they must be obtained from food. Both omega-3 and omega-6 fatty acids contain immune regulatory functions and have a range of benefits for many different immune cells in our body including regulating the production and secretion of cytokines, anti-inflammatory properties, and modulating T cell activation.
Autoimmune conditions such as Hashimoto’s, psoriasis, Crohn’s disease, multiple sclerosis, or rheumatoid arthritis are a sign that the immune system is in overdrive and needs to be healed and rebalanced. Most people with autoimmunity are deficient in the basic nutrients needed to regulate the immune system.
9. Estrogen Dominance
Hormone imbalances can be a root cause of autoimmunity. Excess estrogen is pro-inflammatory and can add “fuel to the fire” of an autoimmune process. Chronic inflammation due to estrogen dominance pushes the immune system balance towards more of a Th17 response, which is at the root cause of tissue destruction in autoimmune diseases.
Stress also impacts hormone balance. Progesterone is a precursor to cortisol and helps balance out the effects of estrogen in the body. However, in chronic stress the demand for cortisol is high, and progesterone can be depleted rapidly. When progesterone runs low, even normal levels of estrogen can be inflammatory because they are not balanced out by progesterone.
Hormonal imbalances that we see in our practice every day are:
- Cortisol or adrenal dysfunction
- Low DHEA
- Estrogen dominance
- Low progesterone
- Androgen imbalances, such as low testosterone or high dihydrotestosterone
- Hypothyroidism
- Insulin resistance
Genetics
Genetics can play a role in autoimmunity, meaning you may have a higher chance of developing autoimmunity if someone in your family has had it. However, this does not mean you will develop an autoimmune disease, part of this has to do with epigenetics (the ability to “turn off” bad genes and “turn on” good ones).
Genes are the blueprints of your immune system and every cell in your body, but your genes are not your destiny. Genes are influenced by environment such as your diet, toxins, stress, hormones, inflammation, and more. It is only when your body is overwhelmed with triggers, that the genes that predispose you to autoimmunity can get turned on and start an autoimmune process. Suddenly you are experiencing an array of symptoms that you didn’t have before because your body is triggered and trying to protect itself.
How Do Functional Medicine Doctors Discover the Root Cause Of an Autoimmune Condition?
- Comprehensive blood chemistry tests including metabolic panel and CBC with differentials
- Iron and anemia panel
- Hormones such as estrogen, testosterone, and insulin
- Complete thyroid panel including Hashimoto’s antibodies (if indicated)
- Comprehensive digestive stool analysis with microbiome testing
- SIBO breath test
- Salivary cortisol and adrenal function
- Nutritional tests measuring vitamins, minerals, antioxidants, healthy fats, or amino acids
- C-reactive protein (hs-CRP)
- Homocysteine and Methylation status
- Vitamin D
- Food sensitivity or food allergy
- Genetic tests
- Organic Acids Test (OATs)
Autoimmunity is not a life sentence. Discover the root causes of your autoimmune disorder or symptoms with a functional medicine practitioner. Root cause care has the potential to heal your immune system with a whole care perspective and allows you to take a personalized and proactive approach to your health and wellness.